INTRODUCTION–

• Commonest vaccine-preventable illness.
• Highly contagious viral infections of respiratory system.
• Characterized by fever ,URTI , generalized maculopapular rash.
• Self limiting course but high morbidity and mortality.
EPIDEMIOLOGY-
A) Measles virus is RNA virus of only one known serotype
Family – Paramyxoviridae
Genus – Morbillivirus
B) Source of infection– Nasopharyngeal secreations of infected clinical/ sub-clinical human case.
C) Transmission– Droplet infection.
D) Incubation period– 08-12 days period.
E) Period of Infectivity– Extends from 4 days before to 5 days after the appearance of rash.
F) High risk factors–
• Pre-school childrens.
• Overcrowding.
• Poor immunization.
• More common in winter or spring season.
• Immunocompromised state.
• Severe malnutrition.
• Vitamin A deficiency.
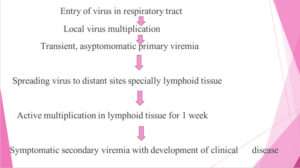
PATHOGENESIS–
CLINICAL MANIFESTATIONS-
3 STAGES
A) Prodromal phase
B) Eruptive phase
C) Convalescent phase
A) Prodromal phase (4-5 days)
Mild to moderate fever
Upper respiratory illness with 3 C i.e cough, corrhyza, conjunctivitis



Koplik spots
• Pathognomic sign of measles
• Appearing 1-4 days prior to onset of rash
• First appear as discrete red lesions with bluish white spots in the centre
• On the inner aspects of cheeks at the level of molars
• May spread to involve the lips hard palate and gingiva.

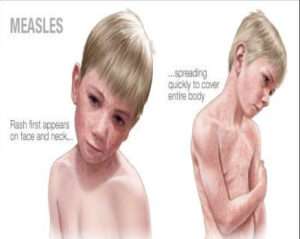
B) ERUPTIVE PHASE (5-7 DAYS) :-
• Skin rashes appear on 4-5th day with transient rise of fever.
• Starting as faint blanching macules, first along the hair-line on the forehead, behind the ears, face and neck
• Then rapidly turn into maculopapular rash and extend downward, involving whole body in next 2-3 days.
• May associated with moderate cervical lymphadenopathy.
• Constitutional symptoms eg. Anorexia, malaise
• GIT upset – eg. Diarrhoea, vomiting or
• Abdominal pain due to mesenteric lymphadenopathy
C) Convalescent phase :-
• Rashes disappear in the same sequence after 5-7 days
• Leaving behind a branny- brown desquamation ( post-measles staining) for next 10-15 days

DIAGNOSIS–
Mainly clinical, based on
A) History of ongoing outbreak and unimmunized child
B) Typical rash after 4th – 5th day of prodromal illness.
C) Presence of kolpik spots for early diagnosis
D) Post- measles staining for retrospective diagnosis.
INVESTIGATIONS-
1] CBC – Leucopenia
lymphocytes more than Neutrophils
Absolute neutropenia.
2] CRP
3] ESR
– Serological findings:-
• IgM antibodies –
Appears 1-2 days after onset of rash, Remains detectable for about 1 month
• IgG antibodies –
4 fold rise in IgG antibodies confirms diagnosis
4] Culture – Blood, Urine, Respiratory secretion
5) Throat swab for PCR test
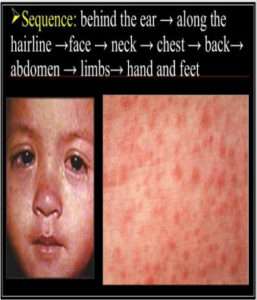
Typical rash of measles-
• Maculopapular often slightly hemorrhagic
• Appears on 4th – 5th day with transient rise of fever
• Rash 1st appears behind the ear, near the hair line of Forehead, face and neck
• Resolution of rash follows same sequence
DIFFERENTIAL DIAGNOSIS-
VIRAL
• German measles
• Roseola Infantum
• Erythema Infectiosum
• Infectious mononucleosis
OTHERS
• Meningococcemia
• Typhoid fever
• Scarlet fever
• Kawasaki syndrome
• Rickettsial fever
• Drug Eruption
MANAGEMENT-
• Supportive
• No specific antiviral therapy approved
• Goals of therapy – 1) Maintenance of hydration
2) Oxygenation
3) Comfort
a) Maintenance of nutrition and hygiene
b) Antipyretic for fever and comfort
c) Airway humidification and supplemental oxygen
d) Treatment of complication
Vitamin A :- • Vit A therapy is indicated for all patients with measles
• Reduces morbidity and mortality in measles
• Correlation between level of retinol and severity of illness DOSE :- 12 months or older – 2 lock IU 6 months to 11 months – 1 lack IU < 6 months – 50,000 IU Once daily for 2 days
PREVENTION–
A) Universal Immunization :-
MMR – Live attenuated vaccine
Dose :- 1st – at age of 9 months
2nd- at age of 15-18 months
B) Post- exposure prophylaxis :-
• Useful to reduce severity duration of illness.
• Should receive within 3-5 days of exposure
• Indicated only in high-risk household contacts
• Unimmunized infants – Immunoglobulins with vaccine
• Older unimmunized children without past History of disease – Only vaccine
• Immunocompromised or pregnant womans – Only Immunoglobulins
C) Isolation :-
• Isolation of case and suspected contacts during Infectivity period
Contributor- Medico Hrishikesh Gawali