Diabetes is a metabolic disease in which there is an increase in blood glucose level, now it has become a lifestyle globe. The disease will lead to several complications like eye related problems, delay in wound healing, heart diseases, kidney diseases, nerve damages and oral problems.
Yes! ORAL PROBLEMS is one of the complications of diabetes, which is usually neglected by the majority of the population.
Diabetes mellitus is a chronic disease resulting from a relative or absolute deficiency of insulin, where it is affecting metabolism of carbohydrate, protein, and fat. The most obvious abnormality is a high level of blood glucose, especially following a meal. Diabetes occurs in two major forms, type I and type II diabetes. Type I diabetes is the result of a reduction in or the elimination of insulin production by beta cells in the pancreas. Type II diabetes is characterized by a deficient response to insulin by target cells, although insulin production is typically normal or even enhanced in these individuals
HOW DIABETES CAN CAUSE ORAL PROBLEMS?
WHAT ARE THE SYMPTOMS?
WHAT ARE THE TREATMENTS?
Oral cavity mainly consists of teeth, tongue, gums, cheeks, salivary glands, hard and soft palate. The oral cavity is always pooled with saliva, which acts as a protective barrier in many conditions and hosts many microorganisms. Due to increased blood glucose level, the activity of microorganisms increases which leads to oral diseases. Diabetes alone doesn’t cause oral related problems, the other local irritants aggravate the condition.
The main oral complications of diabetes are –
• Gum disease or periodontal disease is one of the sixth complications of diabetes, which exhibits as formation of abscess, swelling of gums, receding gums, loosening of teeth, rapid destruction of bone.
• Fungal infections are due to increased multiplication of microorganisms such as candida albicans, and impaired immune system
• Burning mouth is due to other local factors along with diabetes.
• Dry mouth (xerostomia) and bad breath is due to decreased salivary flow which, increases the risk of caries
• Delayed wound healing is due to reduced cell responses (polymorphonuclear chemotaxis)
The other less common complications are –
Dry socket, Trigeminal nerve involvement, Enlargement of salivary glands, Altered taste sensation, Angular cheilitis, Oral lichen planus, Pyogenic granuloma
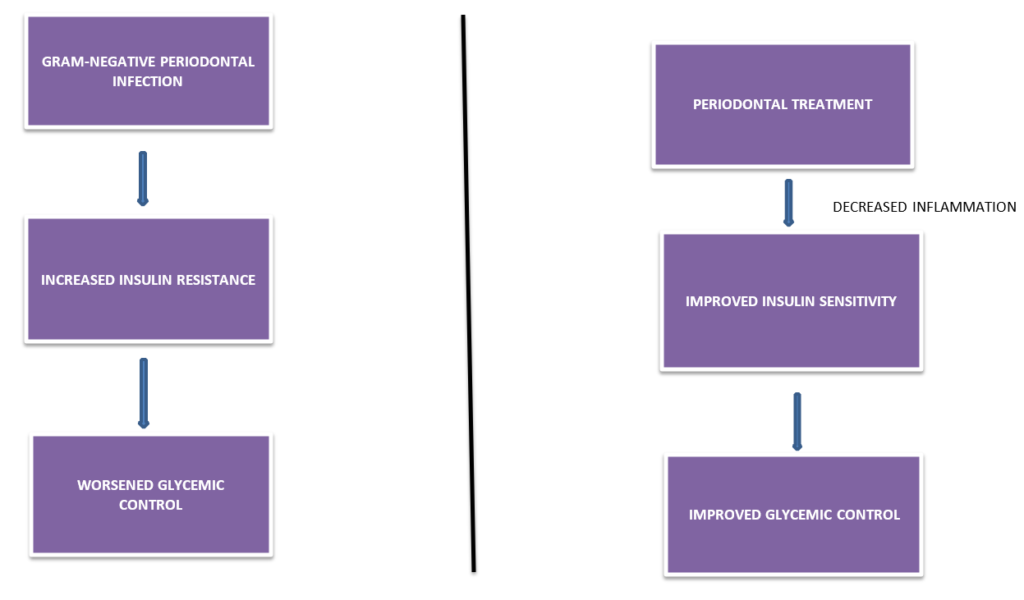
TWO WAY RELATION OF DIABETES –
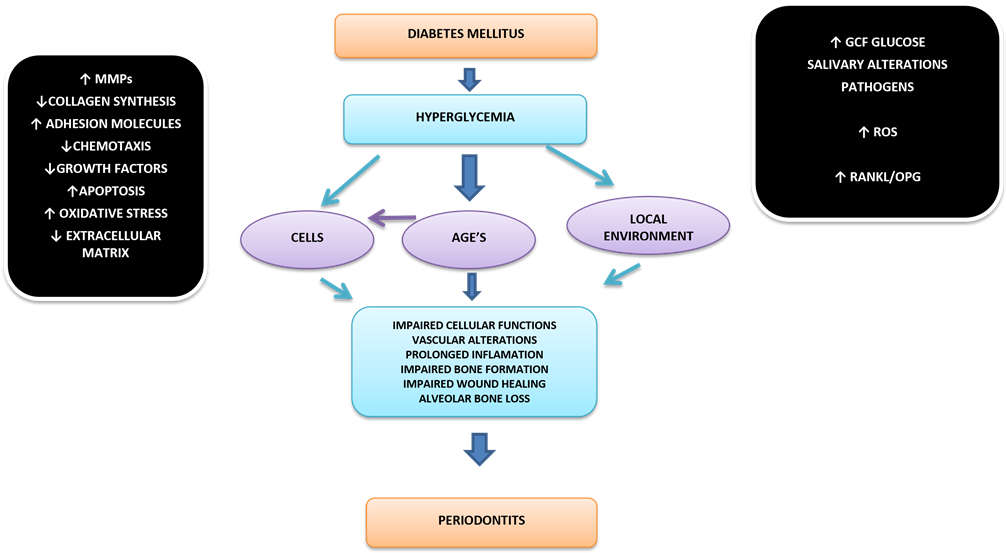
Potential Effects of Periodontal infection And Periodontal Therapy on Glycaemia in Patients with Diabetes
Managements of oral complications of Diabetes –
Many treatments are not different from those recommended for general population without diabetes. However, managing diabetes patients do require more rigorous follow-up, more aggressive interventional therapy rather than observation, regular communication with physicians and greater attention to prevention. Diabetes patients, with a history of poor glycemic control and oral infections, require frequent recall visits and fastidious attention should be given to acute oral infections.
In most cases, the well-controlled type 1 or type 2 diabetic patients can be managed in a manner consistent with the management of a healthy non diabetic person. The periodontal surgical procedures can be performed; although it is important for the patient to maintain a normal diet during the postsurgical phase. The detailed history of diabetic complications should be collected from the patient, to determine the recent test results (eg., glycosylated hemoglobin and postprandial blood glucose levels) and maintain an ongoing dialogue with the patient’s physician. Supportive periodontal therapy should be given at 2 to 3 months intervals because few studies indicates that there is slight tendency to progressive periodontal destruction even after effective metabolic control.
Treatment –
• SUPPORTIVE TREATMENT: Diet control is the most important factor, adapting lifestyle changing habits like regular exercise, walking, yoga , meditation.
• SYMPTOMATIC TREATMENT: Maintaining normal blood glucose levels (non diabetic individual FBS:70- 110mg/dl, PPBS:126 mg/dl, PPBS>200mg/dl). Regular visiting a General physician and a Dentist.
SPECIFIC TREATMENT: Oral hypoglycemic drugs, Insulin,systemic antibiotics, supra and subgingival scaling, root planning, selected tooth extractions, periodontal surgeries, reduction of caries, usage of mouthwash, brushing twice a day.
Contributor- Dr. Kavyashree M Prasad





Helpful
Thank you
Nicely written